Introduction
Sleep apnea is a disorder that affects more than 18 million Indians. The word apnea means pauses in breathing; people who have sleep apnea literally stop breathing for short periods of time while sleeping. The pauses in breath usually last only a few seconds, but a person with sleep apnea may stop breathing many times in an hour, and hundreds of times over the course of a night. Most people with sleep apnea are unaware of their condition.
There are two kinds of sleep apnea: obstructive sleep apnea and central sleep apnea.
Obstructive sleep apnea, the most common type, occurs when parts of the upper airway block breathing at the back of the throat. This blockage can occur when the muscles of the throat relax during sleep.
Central sleep apnea is much less common. It occurs when the brain fails to properly send “breathe” signals to the rest of the body.
The pauses in breath that characterize sleep apnea interfere with the delivery of oxygen to the body. Sleep apnea can lead to mood and memory problems, high blood pressure, heart disease, weight gain, impotence and headaches. Untreated sleep apnea is a potentially life-threatening condition.
Symptoms
Snoring is the most common symptom of sleep apnea. Friends or family members of people with sleep apnea often report hearing very loud snoring. They may also witness pauses of breath and/or gasping or choking episodes. These incidents can be upsetting to family members and may interrupt the sleep of others in the household.
These episodes lead to frequent awakening, which patients often do not remember. Interrupted sleep may lead to extreme fatigue and chronic tiredness, another common symptom of sleep apnea. People with sleep apnea may have difficulty staying awake during the day. They may fall asleep while sitting in a chair watching TV, at work, or even while driving. Sleep apnea has been associated with an increased incidence of motor vehicle incidents.
Other signs and symptoms of sleep apnea include :
- Morning headaches.
- Memory or learning problems.
- Waking up frequently to urinate.
- Dry mouth or sore throat upon awakening.
- Inability to concentrate.
- Feeling irritable or depressed.
- Mood swings or personality changes.
Both adults and children can suffer from sleep apnea. Sleep apnea in children is associated with poor school performance, behavioral problems, and hyperactivity.
Causes
Central sleep apnea is caused by a problem in the brain and generally occurs in people who are seriously ill from other causes. It is sometimes seen in people who have experienced an injury to the brainstem, in people with Parkinson’s disease and in people who have experienced strokes. Sometimes, there is no known cause for central sleep apnea.
Obstructive sleep apnea occurs when something obstructs, or blocks, the airway, interfering with the flow of air to the lungs. Normally, the muscles at the back of the throat keep the airway wide open. During sleep, the muscles of the throat relax, narrowing the airway. Other parts of the upper airway, such as the tonsils and tongue, can then temporarily block the airway.
Risk Factors
Obesity and aging increase the risk of developing sleep apnea. Over half of all people who have sleep apnea are overweight. Sleep apnea is also more common in people over the age of 40, although people of any age can develop sleep apnea.
Sleep apnea seems to run in families, so scientists suspect that genes may play a factor in the development of sleep apnea.
People who have small or unusually-shaped upper airways are more likely to have sleep apnea. Factors that may increase the risk of sleep apnea include large tonsils, significant overbite, or a recessed chin.
Allergies can also restrict airways and increase the risk of sleep apnea.
African-Americans, Pacific-Islanders and Hispanics tend to have more cases of sleep apnea per population than other ethnic groups, but researchers still aren’t sure if race and ethnicity increases the risk of sleep apnea or if other factors are at play.
Smoking and alcohol use increase the risk of sleep apnea.
Complications
By interfering with normal sleep, sleep apnea can affect the entire body.
Pauses in breath during sleep decrease oxygen levels in the body. Decreased oxygen levels trigger the release of stress hormones. While the body can handle this stress on a “sometimes” basis, chronic exposure to stress hormones takes a toll on the body, especially when combined with chronic lack of sleep. Untreated sleep apnea can lead to high blood pressure, irregular heart rhythms (particularly atrial fibrillation), heart failure, heart attack, and stroke.
Sleep apnea can cause heart and circulatory problems, or it can make pre-existing conditions worse. Sleep apnea may make it more difficult to effectively treat high blood pressure.
Preparing for your Appointment
If someone you love exhibits signs or symptoms of sleep apnea, encourage him or her to see a health-care provider. Bed partners usually can describe the frequency and nature of apneas better than the patient. Discuss the symptoms you’ve observed; you may also want to keep a written record of symptoms, including snoring, gasping or choking episodes and daytime tiredness. Some people have even been known to record a partner’s snoring, to provide audio evidence!
If you suspect you have sleep apnea–or if someone expresses concern about your snoring, gasping, or choking at night–schedule an appointment with a health-care provider. Many people put off seeking medical attention, dismissing reports of snoring or trouble breathing as exaggerations or “a big deal about nothing.” But ignoring potential symptoms of sleep apnea can be dangerous.
Be honest: How often are you tired during the day? Have you ever fallen asleep at work? While reading? Behind the wheel?
Keep a sleep diary for a week or two. Include what time you go to bed, how often you wake during the night, how rested you feel in the morning and during the day, and any other sleep problems or symptoms you notice. It may be helpful to have your sleep partner add his or her observations to your sleep diary also.
Compile a list of any medications and supplements you may be taking. (Include the name, dose, and how often you take the medication or supplement.) Double check your family history, as well. Note anyone who has been diagnosed with sleep apnea, as well as anyone who snores regularly or has other sleep difficulties.
Bring your sleep diary, list of medications, and family history with you to your appointment. You may want to bring your sleep partner, as well.
Test & Diagnosis
At your initial appointment, a clinician will take a complete medical history, discuss your signs and symptoms, and give you a physical examination, paying particular attention to your upper airway. Your health-care provider will look in your mouth and nose.
If the clinician suspects that you have sleep apnea, he will refer you for a sleep study. A sleep study, or polysomnogram (PSG), is the definitive diagnostic tool for sleep apnea.
A sleep study uses multiple tools to track your breathing, heart rate, blood pressure, oxygen level, sleep, brain activity, and movement while you sleep. The study takes place overnight.
Many sleep studies occur in a sleep center, which may be located in a hospital or separate, freestanding building. You’ll receive a set of sleep study instructions in advance, which will tell you what time to arrive and what to bring; other instructions, such as “don’t use hair conditioner on the day of your appointment,” may also be included.
A technician will show you to your room, which will probably feature a comfortable bed and look much like a hotel room (with some extra medical equipment). The technician will also apply sensors and wires to your scalp and body. This may take a few minutes, but it’s painless. The technician will help you to bed, attach the sensors to any necessary equipment and tuck you in.
At first, it may seem impossible to sleep while attached to so much equipment, but most people fall asleep with little difficulty. Technicians will track your sleep, breathing, heart rate, movement, oxygen levels, and brain activity while you sleep. They may wake you up periodically during the night, and help you to go to the bathroom while keeping the wires in place.
A sleep specialist will interpret the data from your sleep study to see if you have sleep apnea. You will typically receive the results of your sleep study within a few days of the study.
If your health-care provider strongly suspects sleep apnea, he may order a split-night sleep study. A split-night sleep study is divided into two portions: During the first part, technicians monitor your breathing and body systems during sleep, as during a normal sleep study. If those readings suggest sleep apnea, the second part of the night will be spent seeing how your body responds to treatment for sleep apnea.
Home-based sleep studies may be an option for some people with suspected sleep apnea. A home-based sleep study occurs at home, using a portable device that measures breathing, heart rate, and oxygen levels.
Treatment
Mild cases of sleep apnea can often be treated with lifestyle modifications. If you have mild sleep apnea, your health-care provider may ask you to:
- Avoid alcohol, especially before bed. Alcohol makes you sleepy, and makes it harder for your body to hold your airway open as you sleep.
- Lose weight. If you are overweight or obese, losing a few pounds may make a big difference in your breathing and sleep.
- Sleep on your side. It’s much harder for your airway to become blocked when you’re lying on your side. Some people place or sew tennis balls into the backs of their pajamas, to remind them to roll over if they inadvertently roll onto their backs at night.
- Quit smoking. Smoking increases your risk of severe sleep apnea, and is harmful to your overall health.
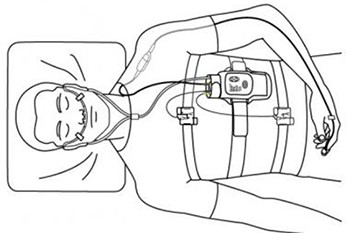
The most common treatment for sleep apnea is continuous positive airway pressure, or CPAP. CPAP uses airway pressure to keep the airway open during sleep. A person using CPAP wears a mask over the nose or nose and mouth at night. The mask is connected via a hose to a portable machine, which sits at the bedside and delivers air pressure. Most CPAP machines can also measure and record oxygen levels during sleep.
CPAP is typically used for moderate to severe cases of sleep apnea. It can take some time to get used to CPAP, but people who try it often feel so much better after just one night of treatment that they quickly embrace the treatment. Don’t give up if CPAP feels strange or uncomfortable at first. Your health-care provider will work with you to minimize side effects (such as dry mouth, stuffy nose, and headaches) and maximize your comfort and sleep.
Other types of positive airway pressure can also be used to hold the airways open during sleep. Bi-level positive airway pressure (BPAP) devices provide more pressure during inhalations and less pressure during exhalations. Expiratory positive airway pressure (EPAP) devices are disposable devices that are placed inside the nostrils each night; a valve inside the device creates pressure when you exhale, holding the airway open.
Other treatments for sleep apnea include:
Oral appliances : Oral appliances are special plastic mouthpieces that gently reposition the lower jaw and tongue so that the airways remain open during sleep. Oral appliances are inserted at bedtime and worn in the mouth throughout the night. They are often used to treat snoring, and can be used to treat some cases of mild to moderate sleep apnea.
Because everyone is different, oral appliances must be custom-made by dentists with advanced training in dental sleep medicine. Your health-care provider can refer you to a qualified dentist, if needed.
Surgery : Surgery is rarely used as a first-line treatment for sleep apnea. Typically, surgery is only considered if other treatment options fail to improve breathing at night.
If overly large tonsils and/or adenoids are causing or contributing to sleep apnea, removal of the tonsils (tonsillectomy) or tonsils and adenoids (tonsillectomy and adenoidectomy) may relieve sleep apnea.
Other surgical options include: Nasal surgery, Sometimes, structural problems inside the nose contribute to sleep apnea. Surgeries such as septoplasty (repair or straightening of the septum, the “wall” between your nostrils) or sinus surgery may improve airflow through the nose.
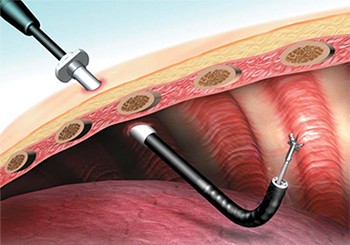
Tissue removal, Some people have excess tissue at the back of their mouths and throats. Removal of this tissue via a surgery called uvulopalatopharyngoplasty (or UPPP) may decrease snoring and relieve sleep apnea.
UPPP is the most common surgical procedure for sleep apnea. It is usually performed in a hospital under general anesthesia and requires an overnight hospital stay.
Surgical implants. Tiny little polyester rods can be implanted into the soft palate at the back of the mouth. These implants “stiffen” up that tissue, making it less likely to block the airway during sleep. The implants can be placed under local anesthesia in a surgeon’s office; the patient is awake during the procedure and anesthetic is used to numb the area. Surgical implants may be an option for people who have mild sleep apnea and can’t tolerate CPAP.
Jaw surgery. Surgically moving the jaw forward may relieve sleep apnea in some patients, especially patients who have small or underdeveloped jaws. This specialized surgery is performed under a general anesthetic in a hospital and requires the skills of specialized surgeons.
Tracheostomy. Rarely, sleep apnea is so severe that surgeons bypass the upper airway completely and cut a hole in the throat to facilitate breathing. This option is only used if all other options have failed and sleep apnea is life-threatening.
Lifestyle & Home Remedies
Healthy sleep habits contribute to a good night’s sleep. Most adults need 7 to 8 hours of sleep per night. Try to go to bed and get up at approximately the same times each day.
Avoid excessive alcohol intake, especially before bed. Alcohol relaxes the muscles of the upper airway and may make sleep apnea worse.
Maintain a healthy weight. Losing excess weight may ease sleep apnea; gaining weight could make your sleep apnea worse.
Don’t smoke. Smoking is harmful to the lungs and increases the risk of severe sleep apnea. If you smoke, quitting will improve your overall health and may relieve your sleep apnea.
See your health-care provider for regular checkups. Your provider will check to see how well your treatment is working and make adjustments to your treatment plan, if necessary.
If you are going to have surgery or undergo a medical procedure that requires medicine to put you to sleep, let your surgeon and health-care providers know that you have sleep apnea. They will carefully monitor your breathing and airway during the procedure.
Other Resources
Sleep apnea can affect everyone in a household. If you (or a partner) have sleep apnea, give the treatment time to work. It may take time to find the most effective treatment, but the entire household will probably sleep better and feel better once the person with sleep apnea is sleeping soundly on a regular basis.
Talking to other people with sleep apnea can also be helpful. Your health-care provider can also answer your questions and address your concerns.