What Abnormal Results Mean
Many disorders can be diagnosed with bronchoscopy, including:
- Infections from bacteria, viruses, fungi, parasites, or tuberculosis.
- Lung damage related to allergy-type reactions.
- Lung disorders in which the deep lung tissues become inflamed and then damaged.
- Lung cancer or cancer in the area between the lungs.
- Narrowing (stenosis) of the trachea or bronchi.
- Sarcoidosis.
- Vasculitis.
- Other inflammatory lung disease.
What does a spirometry tell my doctor?
 Spirometry is a simple breathing test, that can be done in physician’s office that measures the amount of air you can blow out after you have taken in the deepest breath you can. The results of this test give two important numbers that measure airway obstruction.
Spirometry is a simple breathing test, that can be done in physician’s office that measures the amount of air you can blow out after you have taken in the deepest breath you can. The results of this test give two important numbers that measure airway obstruction.
FVC – Forced Vital Capacity : the total volume of air you can forcefully blow out. It is an assessment of the size of your lungs, how well your lungs expand and contract, and how well the air passages open and close.
Patients with obstructive lung disease usually have a normal or only slightly decreased vital capacity. A Reduced FVC is associated with restrictive lung disorders, diseases that may be caused by inflammation or scarring of the lung tissue (interstitial lung disease) or by abnormalities of the muscles or skeleton of the chest wall.
FEV1 – Forced Expiratory Volume : is the volume of air that you can blow out in the first second of exhalation.
Typically FEV1 is considered “normal” if greater than 80% of predicted. FEV1 is reduced in both obstructive and restrictive lung disease.
FEV1/FVC : This ratio compares the volume of air expelled in the first second to the total volume expelled.
In healthy patients the FEV1/FVC is usually around 70%-80%. In patients with obstructive lung disease FEV1/FVC decreases and can be as low as 20-30% in severe obstructive airway disease. Restrictive disorders have a near normal FEV1/FVC ratio.
What you need to do before the test?
- Wear comfortable clothing.
- Ideally you should not use your inhalers before your spirometry. There are different types of bronchodilators; some are long acting and others are short acting inhalers so ask your doctor how long you should avoid using your inhaler/s before the test.
- If you experience breathing problems before your test, go ahead and use your inhaler/s. Inform the person performing the test the name of the inhaler/s you used, dosage/puffs taken, and the time you used them.
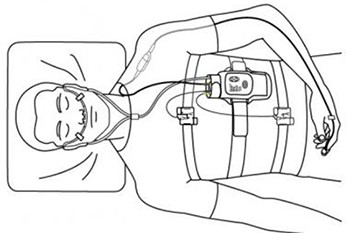
What happens during the test?
- You will be asked several questions (listed below) that will be used to determine what ‘normal’ lung values would be for you if your lungs were healthy.
- Age : lung function declines with age.
- Height : taller people have larger lungs.
- Sex: women have smaller lung volumes.
- You will be asked to sit up straight and uncross your legs or to stand up.
- Often you will have a nose plug placed on your nose.
You will be instructed to :
- Take in a big breath.
- Place the mouthpiece into your mouth and seal your lips tightly around the mouthpiece.
- Blast your air into the mouthpiece as hard and fast as you can, squeezing out all the air in your lungs.
- Keep on blowing out the same breath until you are told to stop.
- To make sure you understand the directions ask the technician to demonstrate the procedure.
- The test will be repeated several time to make sure that the measurements are correct.
- The spirometry may be repeated after you receive a bronchodilator inhaler or nebulizer.
 What is LAVAT?
What is LAVAT?
Medical thoracoscopy, or local anaesthetic video assisted thoracoscopy (LAVAT) is a day procedure, performed in the hospital, to allow further assessment of pleural fluid collections and pleural diseases.
What is Involved?
- LAVAT is often performed under conscious sedation.
- Admission to hospital may be required depending upon whether a pleurodesis is performed, or complications (which are rare) occur.
Medical thoracoscopy was initially performed in 1910 by an internist from Sweden, Hans-Christian Jacobaeus. Jacobaeus was the first to use the term thoracoscopy, which he described as “replacing fluid with air” in order to examine the pleural surfaces of two patients with tuberculous pleurisy. Jacobaeus later developed a therapeutic application for thoracoscopy by using thermocautery to lyse adhesions and create a pneumothorax to treat tuberculosis.
During the 1950s and 1960s, thoracoscopy gained popularity with pulmonologists because of the tuberculosis endemic in the United States. The major indications were for pleural and pulmonary biopsies for diffuse lung disease. However, with the advent of effective chemotherapy for tuberculosis, the need for thoracoscopy decreased. The procedure was later adopted by surgeons after advances in optics, laparoscopic techniques, and video technology. Thoracoscopy grew into the video-assisted thoracoscopic surgery that is currently performed by thoracic surgeons.
The term thoracoscopy is confusing because it refers to both the medical and surgical procedures. To avoid confusion, some authors suggest that medical thoracoscopy should be referred to aspleuroscopy. The term thoracoscopy may be used exclusively for the surgical thoracoscopic procedure.
What you need to do before the test
- Comfortable clothing should be worn.
- Wear shoes that are comfortable to walk in , such as tennis shoes.
- You may use your usual walking aids during the test (cane, walker, etc.).
- Take your medications as prescribed.
- You may eat a light meal before early morning or early afternoon tests.
- Do not exercise vigorously within 2 hours of beginning the test.
What happens during this test?
You will be asked to familiarize yourself with the Modified Borg Scale (See Borg Scale listed below). This scale is way of rating your degree of breathlessness and/or difficult, uncomfortable or labored breathing as well as fatigue level. You will be asked to use the Borg Scale before, during and after your walk.
What is pneumonia?
Pneumonia is caused by an infection in the lungs. The infection affects the air sacs in the lungs rather than the tubes that carry air to and from the lungs. Infected parts of the lung fill up with fluid, which contains white blood cells that fight the infection.
What causes pneumonia? Where does it come from?
Pneumonia is caused by germs (tiny organisms that can cause disease). Viruses, bacteria and fungi are types of germ that can cause pneumonia. Healthy people don’t usually have these germs in their lung tissue. Germs sometimes get to the lung through our bloodstream, but most often they reach the lung tissue inside tiny droplets of water in the air that we breathe in. Usually, these germs come from other people, who spread them by coughing and sneezing out the droplets of water containing the germs.
Sometimes, the germs come from more unusual places. Legionnaires’ disease is a type of pneumonia caused by germs that thrive in very warm water. The germs that cause psittacosis are usually caught from birds, especially parrots. MRSA is often found in hospitals and can cause pneumonia in people who are admitted to hospital for other reasons.
What is tuberculosis (TB)?
Tuberculosis (TB) is a disease caused by bacteria that are spread from person to person through the air. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine. In most cases, TB is treatable and curable; however, persons with TB can die if they do not get proper treatment.
What is multidrug-resistant tuberculosis (MDR TB)?
Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These drugs are used to treat all persons with TB disease.
What is extensively drug resistant tuberculosis (XDR TB)?
Extensively drug resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Because XDR TB is resistant to the most potent TB drugs, patients are left with treatment options that are much less effective. XDR TB is of special concern for persons with HIV infection or other conditions that can weaken the immune system. These persons are more likely to develop TB disease once they are infected, and also have a higher risk of death once they develop TB.
How is TB spread?
Drug-susceptible TB and drug-resistant TB are spread the same way. TB bacteria are put into the air when a person with TB disease of the lungs or throat coughs, sneezes, speaks, or sings. These bacteria can float in the air for several hours, depending on the environment. Persons who breathe in the air containing these TB bacteria can become infected.
TB is not spread by
- Shaking someone’s hand.
- Sharing food or drink.
- Touching bed linens or toilet seats.
How does drug resistance happen?
Resistance to anti-TB drugs can occur when these drugs are misused or mismanaged. Examples include when patients do not complete their full course of treatment; when health-care providers prescribe the wrong treatment, the wrong dose, or length of time for taking the drugs; when the supply of drugs is not always available; or when the drugs are of poor quality.
Who is at risk for getting MDR TB?
Drug resistance is more common in people who :
- Do not take their TB medicine regularly.
- Do not take all of their TB medicine as told by their doctor or nurse.
- Develop TB disease again, after having taken TB medicine in the past.
- Come from areas of the world where drugresistant TB is common.
- Have spent time with someone known to have drug-resistant TB disease.
How can MDR TB be prevented?
The most important thing a person can do to prevent the spread of MDR TB is to take all of their medications exactly as prescribed by their health care provider. No doses should be missed and treatment should not be stopped early. Patients should tell their health care provider if they are having trouble taking the medications. If patients plan to travel, they should talk to their health care providers and make sure they have enough medicine to last while away.
Health care providers can help prevent MDR TB by quickly diagnosing cases, following recommended treatment guidelines, monitoring patients’ response to treatment, and making sure therapy is completed.
Another way to prevent getting MDR TB is to avoid exposure to known MDR TB patients in closed or crowded places such as hospitals, prisons, or homeless shelters.
What will you learn in Pulmonary Rehabilitation?
The education part of the program happens both in a classroom, one-on-one with the professional staff, and during each exercise session.
During group meetings, you will learn new ways to breathe during stressful times and while being active. You will practice these new breathing techniques during your exercise sessions.
You will learn about your medications; what the medications do and how to use your inhalers to get the most benefit from them.
During the program, you may be given an Action Plan that outlines what you should do when you are having a lung flare-up (exacerbation). Some people with breathing problems need to use oxygen.
During pulmonary rehabilitation you will be tested at rest and with exercise to see if oxygen may help you. You will learn the reasons why some people with shortness of breath use oxygen and others do not need it.
If you smoke, the program will provide support for you to quit or get you a referral to a program that can help you to quit.
You will also learn how and when to call you health care provider, including what key points to share with them and what questions to ask.
Also during the program, you can expect to meet others that also have breathing problems. You will have the time to share concerns and successes with others living with lung disease.
What will you do in the exercise sessions?
You may not think that you can exercise when just walking across the room makes you breathless. There are however, standard exercises that have been found to work well for people with breathing problems. The type and amount of exercise you will do will depend on what you can do now and as you get stronger, your exercises will increase. Exercise sessions begin with stretching exercises or warm ups, followed by exercises for your arms and legs. Usually you will do both exercises to build your strength and exercises to build your endurance (stamina). To build your strength, generally weights and lifting devices are used. For endurance, activities might include walking on a treadmill or in a corridor and using a stationary cycle. The amount of time you exercise depends on what you can handle. After attending pulmonary rehabilitation, patients are frequently amazed at how much they can exercise and how much less short of breath they are.
How do Vaccines Work
Immunization (vaccination) is a way to trigger your immune system and prevent serious, life-threatening diseases. Immunization exposes you to a very small, very safe amount of the most important diseases you are likely to encounter at some point in your life.
This mild exposure helps your immune system recognize and attack the disease efficiently. If you are exposed to the full-blown disease later in life, you will either not become infected or have a much less serious infection. This is a natural way to deal with infectious diseases.
Who Should Get the Flu Shot?
In general, anyone who wants to reduce their chances of getting the flu can get vaccinated. However, certain people should get vaccinated each year. They are either people who are at high risk of having serious flu complications or people who live with or care for those at high risk for serious complications. People who should get vaccinated each year are.
People who should get vaccinated each year are:
- People at high risk for complications from the flu.
- People 65 years and older.
- People who live in nursing homes and other long-term care facilities that house those with long-term illnesses.
- Adults and children 6 months and older with chronic heart or lung conditions, including asthma.
- Adults and children 6 months and older who needed regular medical care or were in a hospital during the previous year because of a metabolic disease (like diabetes), chronic kidney disease, or weakened immune system (including immune system problems caused by medicines or by infection with human immunodeficiency virus [HIV/AIDS]).
- Children 6 months to 18 years of age who are on long-term aspirin therapy. (Children given aspirin while they have influenza are at risk of Reye syndrome.);
Women who will be pregnant during the influenza season. - All children 6 to 23 months of age.
- People with any condition that can compromise respiratory function or the handling of respiratory secretions (that is, a condition that makes it hard to breathe or swallow, such as brain injury or disease, spinal cord injuries, seizure disorders, or other nerve or muscle disorders.)
- People 50 to 64 years of age. Because nearly one-third of people 50 to 64 years of age in the United States have one or more medical conditions that place them at increased risk for serious flu complications, vaccination is recommended for all persons aged 50 to 64.
- People who can transmit flu to others at high risk for complications. Any person in close contact with someone in a high-risk group (see above) should get vaccinated. This includes all health-care workers, household contacts and out-of-home caregivers of children 6 to 23 months of age, and close contacts of people 65 years and older.
Immunizations – Pneumonia
What is Pneumococcal Pneumonia?
Pneumococcal disease is a serious disease that cause much sickness and death. It’s a type of bacteria called Streptococcus pneumonia and when these bacteria invade the lungs, they cause the most common kind of bacterial pneumonia and can then invade the bloodstream (bacteremia) and/or the tissues and fluids surrounding the brain and spinal cord (meningitis).
The vaccine prevents 23 types of “strep” infection – including pneumonia, bacteremia and meningitis that can cause death or serious health problems, particularly in older adults.
What Are the Signs and Symptoms?
Pneumococcal pneumonia (begins with high fever, cough, and stabbing chest pains), bacteremia, and meningitis.
Complications
This infection kills thousands of people in the United States each year, most of them under two years of age or over 65 years. Over half a million cases of pneumonia and 60,000 deaths were reported in 2002.
How do you get it?
Pneumococcus is in many people’s noses and throats. Why it suddenly invades the body and causes disease is unknown.
How to prevent it?
Pneumococcal vaccine is very good at preventing severe disease, hospitalization, and death. However it is not guaranteed to prevent all symptoms in all people.
As an adult, do I need it?
You should get the pneumococcal vaccine if:
- You are 65 years old or older.
- You have a serious long-term health problem such as heart disease, sickle cell disease, alcoholism, leaks of cerebrospinal fluid, lung disease (not including asthma), diabetes, or liver cirrhosis.
- Your resistance to infection is lowered due to Hodgkin’s disease; multiple myeloma; cancer treatment with x-rays or drugs; treatment with long-term steroids; bone marrow or organ transplant; kidney failure; HIV/AIDS; lymphoma, leukemia, or other cancers; nephrotic syndrome; damaged spleen or no spleen.
- You are an Alaskan Native or from certain Native American populations.
How Do Vaccines Work
Immunization (vaccination) is a way to trigger your immune system and prevent serious, life-threatening diseases. Immunization exposes you to a very small, very safe amount of the most important diseases you are likely to encounter at some point in your life.
This mild exposure helps your immune system recognize and attack the disease efficiently. If you are exposed to the full-blown disease later in life, you will either not become infected or have a much less serious infection. This is a natural way to deal with infectious diseases.