Pulmonary rehabilitation is a multi-disciplinary approach involving a Pulmonologist, a physiotherapist, a dietician and a psychologist.
It is a rehabilitation programme for patients with chronic respiratory diseases with moderate to severe respiratory impairment.
A rehabilitation programme is individually tailored for every patient keeping is disease severity and his needs in mind.
What will you learn in Pulmonary Rehabilitation?
The education part of the program happens both in a classroom, one-on-one with the professional staff, and during each exercise session.
During group meetings, you will learn new ways to breathe during stressful times and while being active. You will practice these new breathing techniques during your exercise sessions.
You will learn about your medications; what the medications do and how to use your inhalers to get the most benefit from them.
During the program, you may be given an Action Plan that outlines what you should do when you are having a lung flare-up (exacerbation). Some people with breathing problems need to use oxygen.
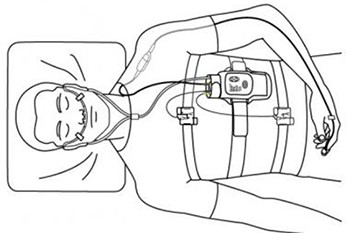
During pulmonary rehabilitation you will be tested at rest and with exercise to see if oxygen may help you. You will learn the reasons why some people with shortness of breath use oxygen and others do not need it.
If you smoke, the program will provide support for you to quit or get you a referral to a program that can help you to quit.
You will also learn how and when to call you health care provider, including what key points to share with them and what questions to ask.
Also during the program, you can expect to meet others that also have breathing problems. You will have the time to share concerns and successes with others living with lung disease.
What will you do in the exercise sessions?
You may not think that you can exercise when just walking across the room makes you breathless. There are however, standard exercises that have been found to work well for people with breathing problems. The type and amount of exercise you will do will depend on what you can do now and as you get stronger, your exercises will increase. Exercise sessions begin with stretching exercises or warm ups, followed by exercises for your arms and legs. Usually you will do both exercises to build your strength and exercises to build your endurance (stamina). To build your strength, generally weights and lifting devices are used. For endurance, activities might include walking on a treadmill or in a corridor and using a stationary cycle. The amount of time you exercise depends on what you can handle. After attending pulmonary rehabilitation, patients are frequently amazed at how much they can exercise and how much less short of breath they are.
Effects of pulmonary rehab
Pulmonary rehabilitation, as an adjunct to standard medical therapy, may result in improvement in some of these areas.
Relief of Symptoms
Dyspnoea and fatigue are hallmark symptoms in most COPD patients. There is a considerable body of evidence that pulmonary rehabilitation improves exertional dyspnoea [3, 13] and dyspnoea associated with daily activities in COPD [2, 4, 6, 8-11, 14].
Improvement in Exercise Tolerance
Pulmonary rehabilitation improves exercise ability in COPD [4-11, 14-16]. Favourable outcomes include increases in maximal exercise tolerance, peak oxygen uptake, endurance time during submaximal testing, functional walking distance, and peripheral and respiratory muscle strength.
Improvement in health status
Pulmonary rehabilitation results in a significant improvement in disease-specific and general measures of health status [4, 6, 9, 14, 17]. These effects are relatively long lasting and not necessarily related to improvements in exercise ability. Multiple domains of health status usually show improvement, such as dyspnoea, fatigue, emotional function and mastery components of the Chronic Respiratory Disease Questionnaire or symptoms, activity and impact components of the St. George’s Respiratory Questionnaire. Improvement in health status following rehabilitation usually exceeds the thresholds for minimum clinically important differences established for respiratory-specific health status questionnaires [18].
Prevention of Complications and Exacerbations
There are conflicting reports on the effect of pulmonary rehabilitation on healthcare service utilisation. A randomised, controlled trial of pulmonary rehabilitation in California failed to show a beneficial effect on hospitalisations in COPD [11]. However, a study of outpatient pulmonary rehabilitation in Wales demonstrated that the rehabilitation group had a similar frequency of hospitalisations but a smaller number of hospital days than a control group in the year following the intervention (10.4 versus 21.0 days) [10]. The reduction in hospital days for both respiratory illness and all causes was noted. In a subsequent cost/utility analysis, these authors demonstrated that outpatient rehabilitation produces cost-per-quality adjusted life-year ratios within bounds considered to be cost effective and resulted in financial benefits to the health service [19].
Effect on Mortality
Limited data from prospective studies do not support the conclusion that pulmonary rehabilitation affects long-term survival [8, 11]. These studies, however, are relatively small and probably were not sufficiently powered to detect this possible effect. In one clinical trial, nutritional intervention, which is commonly incorporated into a comprehensive pulmonary rehabilitation programme, was associated with improved survival rates in a single clinical trial [20].
Effect on Disease Progression
Pulmonary rehabilitation has no significant effects on forced expiratory volume in one second and presumably does not attenuate the decline of airflow limitation in COPD. However, using a broader concept of disease progression, which includes symptoms, exercise capacity, health status and healthcare utilisation, pulmonary rehabilitation would then be considered to have marked effectiveness.
Who requires pulmonary rehab?
Pulmonary rehabilitation should be considered for patients with COPD who have dyspnoea or other respiratory symptoms, reduced exercise tolerance, a restriction in activities because of their disease, or impaired health status (see Definition, diagnosis and staging).
There are no specific pulmonary function inclusion criteria that indicate the need for pulmonary rehabilitation, since symptoms and functional limitations, not the severity of the underlying physiology, direct the need for pulmonary rehabilitation. Often, referral to pulmonary rehabilitation is delayed until patients reach a stage of advanced lung disease. While these patients still stand to derive considerable benefit from pulmonary rehabilitation [21], referral at an earlier stage would allow for earlier preventative strategies, such as smoking cessation, nutritional therapy and a greater latitude in the exercise prescription.
Current cigarette smokers are reasonable candidates for pulmonary rehabilitation and probably obtain similar benefits as nonsmokers or exsmokers. Smoking cessation intervention is an obviously important component of the pulmonary rehabilitation process for smokers.
Components of pulmonary rehab
Comprehensive pulmonary rehabilitation generally includes exercise training, education, psychosocial and behavioural intervention, nutritional therapy and outcome assessment.
Exercise Training
Exercise training is an essential component of pulmonary rehabilitation. In general, two types of exercise training can be given: endurance (or aerobic) training and strength training (see ATS Statement on Pulmonary Rehabilitation).
Endurance training involves dynamic activity of large muscles, usually performed three to four times a week for 20-30 minper session at an intensity of ≥50% of maximal oxygen consumption. This induces structural and physiological adaptations that provide the trained individual with improved endurance for performance of high-intensity activity.
Lower extremity training is the mainstay of endurance training, although there is scientific rationale for incorporating upper extremity training. The optimal training duration for exercise training in COPD has not been established. Most programmes include exercise sessions of ≥30 min, two to five times a week, for 6-12 weeks. The effect of exercise training on exercise capacity and exertional dyspnoea in COPD is dose dependent [22]. However, many patients have difficulty sustaining prolonged high intensity (80% of maximum power output) for prolonged periods [23]. Despite this, lower intensity exercise training is at least as good as high intensity training in improving health-related quality of life [23, 24]. Interval exercise training (repeated periods of near-maximal exercise alternating with short intervals of rest) may give similar benefits as continuous training, but has less associated dyspnoea [25, 26].
Strength training has proven benefits in pulmonary rehabilitation and can be considered supplemental to endurance training [27-29]. While endurance training of the peripheral muscles is of proven benefit in COPD, ventilatory muscle training is also frequently given. While this probably improves respiratory muscle strength, its effect on symptoms and functional limitation has not yet been firmly established [30].
Education
Education is considered an important component of comprehensive pulmonary rehabilitation and is integrated into virtually all programmes. Because of this, its effect in isolation cannot be readily determined. Among the potential benefits of education are: active participation in healthcare [31, 32], increased coping skills [33, 34], a better understanding of the physical and psychological changes of chronic illness, more skill in collaborative self-management and better adherence to the treatment plan [35]. In addition to standard didactic sessions, education may also incorporate breathing strategies, such as pursed-lip and diaphragmatic breathing, energy conservation and work simplification, and advance directives (see Ethical and palliative care issues).
Psychosocial and Behavioural Intervention
Anxiety, depression and difficulties in coping with chronic disease are common in COPD patients and contribute to morbidity.
Psychosocial and behavioural intervention in pulmonary rehabilitation may include educational sessions or support groups focusing on specific problems such as stress management, or instruction in progressive muscle relaxation, stress reduction and panic control [36].
Informal discussions during rehabilitation sessions of symptoms, concerns and problems common to COPD patients may be beneficial. Participation by family members or friends in pulmonary rehabilitation support groups is encouraged. Motivation for pulmonary rehabilitation, which may be suboptimal at the onset, might improve during therapy.
Individuals with major psychiatric conditions should be referred to appropriate professionals.
Nutritional Therapy
Weight loss and muscle wasting, which are present in 20-35% of patients with stable COPD, contribute to morbidity and mortality in COPD, independent of the pulmonary physiological abnormality [20]. Nutritional intervention should be considered for these individuals, especially under conditions of increased exercise-related energy expenditure.