Introduction
There are more than 300 different conditions that are classed as interstitial lung diseases. Most are very rare; but the more common interstitial lung diseases include:
- Idiopathic Pulmonary Fibrosis.
- Sarcoidosis.
- Non-Specific Interstitial Pneumonia .
- Extrinsic allergic alveolitis (also known as hypersensitivity pneumonitis).
- Interstitial lung disease associated with connective tissue disease.
- Pneumoconiosis.
- Interstitial lung disease caused by certain drugs used to treat other conditions.
 Some interstitial lung diseases, particularly sarcoidosis, also affect other organs in the body.
Some interstitial lung diseases, particularly sarcoidosis, also affect other organs in the body.
Research into the prevalence of interstitial lung diseases is difficult as specific diagnoses are not always obtained . Some studies suggest that when cases of idiopathic pulmonary fibrosis and sarcoidosis are added together, they account for 50% of all interstitial lung diseases.
Experts class interstitial lung diseases into two groups: diseases that have a known cause and those where the cause and origin of the disease is unknown.
Symptoms
Interstitial lung diseases usually have a gradual onset. Most people with interstitial lung diseases experience breathlessness and have a decreased ability to do exercise. Other symptoms may include a persistent cough which is usually dry (i.e. without producing phlegm); in advanced disease there may be blue or purple discolouration especially of lips, hands and feet (due to very low oxygen in the blood) and clubbing, or swelling, of the fingers.
Causes
 Only about one in three cases of interstitial lung diseases has a known cause. Experts believe that a combination of genetics, which make people susceptible to the condition, and environmental factors may explain the development of some conditions, including sarcoidosis. Environmental factors have been recognised in 35% of people with interstitial lung disease.
Only about one in three cases of interstitial lung diseases has a known cause. Experts believe that a combination of genetics, which make people susceptible to the condition, and environmental factors may explain the development of some conditions, including sarcoidosis. Environmental factors have been recognised in 35% of people with interstitial lung disease.
Pneumoconiosis is due to inhaled agents in the workplace, which provoke widespread scarring and hardening (fibrosis) of the lungs. The classical causes are silica dust (silicosis), coal dust (coal workers’ pneumoconiosis) and asbestos (asbestosis). These conditions have become less common due to changes in industrial practices.
Extrinsic allergic alveolitis is due to an allergic reaction to any of several inhaled organic agents; the more common causes include exposure to the dust from mouldy hay (farmer’s lung) or from pigeons or caged birds (bird fancier’s lung).
Certain drugs taken as medication for other conditions can also cause interstitial lung disease. The most common examples are: amiodarone (used to treat an irregular heartbeat), bleomycin (a chemotherapy drug), methotrexate (used to treat arthritis) and nitrofurantoin (used to treat urine infections).
Prevention
Prevention of interstitial lung diseases can only be achieved when the cause is known. In these cases avoiding exposure to the relevant environmental risk factor is the best method of prevention.
In the future, experts hope to be able to identify which people are more susceptible to developing an interstitial lung disease as this will help them provide individual preventative measures for each person.
Management
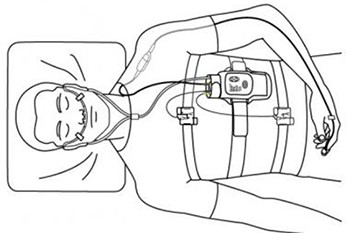
Essential investigations include imaging of the lungs by chest radiography and computed tomography (CT) scanning. Typical appearances of interstitial lung disease include widespread fine nodules, a net-like pattern or a general haziness. High resolution CT scans can be used to help define the specific type of interstitial lung diseases by looking at the type and spread of the lung shadowing on the image.
In advanced lung fibrosis the lungs may have a ‘honeycomb’ appearance due to extensive destruction of the alveoli and development of small cystic spaces within the lung.
Lung function testing including Spirometry And Diffusion capacity of Lungs, 6 MWT and oxygen levels in the blood are also important for diagnosis and monitoring progress of interstitial lung disease.
A surgical lung biopsy, where samples of lung tissue are removed and examined, is sometimes performed for accurate diagnosis of interstitial lung disease but its use has declined as the quality of CT scans has improved.
Treatment of interstitial lung disease depends on the type of ILD. Drugs used are anti-fibrotic and anti-inflammatory drugs. These are most likely to be effective in sarcoidosis, extrinsic allergic alveolitis and some of the rare ILDs but often they have little effect in others such as idiopathic pulmonary fibrosis. Further in the course of the disease oxygen and pulmonary rehabilitation programmes may be required. Despite treatment, some forms of interstitial lung disease worsen progressively and lung transplantation may be required.
Survival times with the different diseases vary greatly. Research has shown that at 5 years after the first diagnosis, 20% of people idiopathic pulmonary fibrosis are still alive whereas 80-100% of people with some forms of hypersensitivity pneumonitis or sarcoidosis are still alive.