Introduction
Asthma is a chronic lung disease that causes wheezing, breathlessness, chest tightness and coughing. It can affect adults or children. Approximately 1 in 12 adults and 1 in 11 children have asthma.
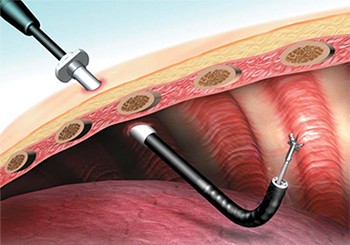
Air enters your body through your nose and mouth. When you breathe air in, it moves down to your lungs through a breathing tube called the trachea (wind pipe) and many branching tubes called airways. In most healthy people, these airways are wide open, so air can flow unobstructed. In people with asthma, the airways are often swollen and irritable.
An “asthma attack” occurs when things that don’t bother most people—so-called “triggers” such as cold, mold, exercise, or pet dander–enter and irritate the airways, which produce extra mucus and swell even more in an attempt to keep the trigger out. The result is swollen and constricted airways filled with mucus. It’s hard for air to move through constricted, swollen, mucus-filled airways. And because the air can’t move freely, it’s difficult to breathe. The wheezing sound that often accompanies asthma is air trying to move through obstructed airways.
While there’s no known cure for asthma, most people with asthma can control their symptoms, so they can breathe freely and live active, healthy lives.
Symptoms
Most people think of wheezing and difficulty breathing when they think of asthma. But these asthma symptoms aren’t always obvious. Coughing that lasts for days or weeks is often the first sign of asthma.
The most common signs and symptoms of asthma include :
Wheezing : Wheezing can range from hard-to-notice to hard-to-miss. You might hear wheezing during daily life, or only at certain times, such as when exercising, when sick, or when exposed to certain triggers. Many people wheeze more at night.
Cough : A cough that occurs frequently, especially in the absence of cold symptoms, may be a sign of asthma. Someone who coughs often but doesn’t have a runny nose or congestion may have asthma. Coughing at night or during or after exercise can also be a sign of asthma.
Shortness of Breath : Feeling like you can’t get enough air is a classic symptom of asthma. Most people with asthma do not feel short of breath all the time; struggling to breathe may be a “sometimes” event.
Chest Tightness : Many people with asthma report feeling chest tightness, especially during cold weather or exercise. Chest tightness is often the first sign of an asthma attack.
You do not have to have all of these symptoms to have asthma. If you have one (or more) of these symptoms on a regular basis, see your doctor immediately. [quite few have associated symptoms due to nose, eye or skin allergy].
Causes
No one knows what exactly causes asthma. Researchers and health-care providers know a lot about what causes asthma attacks, but no one knows why some people get asthma and others don’t.
Most clinicians think that multiple factors contribute to the development of asthma. Here are some things that seem to increase the likelihood that someone will have asthma:
Genes : Asthma may run in families, so scientists think certain genes must be related to asthma. Scientists are conducting research to learn more about how genes can cause asthma.
Environment : Exposure to allergens (things that trigger allergies), certain chemicals and irritants during childhood seem to increase the likelihood that someone will develop asthma. Researchers think that exposure to these materials may affect the immune system, making the person more prone to allergies and asthma.
Exposure to air pollution and lung irritants may also contribute to the development of asthma.
Respiratory Infections : Some infections that occur in early childhood can damage the developing airways and lungs and may contribute to the development of asthma. In people with asthma, colds and other respiratory infections may make symptoms worse.
Risk Factors
Having a family history of asthma or allergies increases the chance that you might have asthma; so does smoking or breathing in tobacco smoke. You can’t change your family history, but you can control your exposure to smoke. Understanding asthma risk factors may help you prevent or minimize asthma.
The most common risk factors for asthma are :
Family history of asthma : If your mother or father has asthma, you’re three to six times more likely to develop asthma than someone who doesn’t have a parent with asthma. As many as three-fifths of all asthma cases may be inherited.
Allergies : Asthma and allergies seem to go hand-in-hand. If you (or a close family member) have allergies, be on the lookout for signs and symptoms of asthma. Not everyone who has allergies develops asthma, but many people with allergies do. Eczema is also associated with asthma.
Smoking/Tobacco Exposure : Both smoking and exposure to secondhand smoke increases the risk of asthma. Children who are exposed to secondhand smoke when they are young are more likely to develop asthma. Teens who smoke are more likely to develop asthma. And adults who are exposed to tobacco smoke at home or at work have a 40% – 60% increased risk of developing asthma compared with adults who aren’t exposed to smoke.
Pollution : Regularly breathing in polluted air–either indoors or outdoors–increases the risk of developing asthma. Studies show that kids who live in heavily polluted areas and near highways are more likely to develop asthma.
Obesity : Asthma is more common in overweight adults and children. Keeping your weight normal and staying away from cigarettes and smoke are two steps everyone can take to minimize the risk of asthma.
Complications
Sometimes asthma gets so bad that it’s next to impossible to get enough air. When asthma is this severe, emergency medical treatment is required.
Asthma left untreated can also permanently damage the airways.
Asthma can interfere with your enjoyment of life. Common asthma complications include lack of sleep (due to asthma symptoms at night, such as coughing) and decreased ability to exercise, play sports, or be active.
Preparing for your Appointment
You know your body better than anyone. The information you give to your providers will help them develop an asthma treatment and control plan just for you.
Before your appointment, keep track of your breathing. Are there certain activities that seem to trigger an asthma attack or make it difficult to breathe? Do you have a hard time breathing at work, but feel fine at home? Write it all down. The more information you give, the better.
Your clinician will want to know what symptoms you have, when they started, and how often you experience them. You’ll be asked about your medical history and family history too, so if you don’t know a lot about your family history, ask an older relative if there’s any history of breathing, lung problems, or allergies in the family.
Make a list of all medications, supplements, and vitamins that you take. Better yet: bring the bottles with you to your appointment. That way, your clinician can see exactly what you’re taking, and in what doses.
If you’re already being treated for asthma, be prepared to tell the doctor how things are going. How often are you taking your medication? How often do you use an inhaler? If you’ve been tracking your lung function, bring that information along too.
Test " Diagnosis
No one test can tell you if you have asthma. You’ll probably be asked a lot of questions, be examined, and have some tests to see if you have asthma.
Because many other things can cause difficulty breathing, a clinician will carefully examine your upper airway by looking in your nose and mouth and will listen to your lungs with a stethoscope.
Doctors can measure how well your lungs are working with a test called spirometry. This test doesn’t hurt at all; all you have to do is breathe out into a mouthpiece that’s attached to a spirometer, a device that measures the amount and speed of air you blow out. Your clinician might measure your lung function before and after activity, to see if it changes. If your test shows reduced lung function, you may be asked to inhale an asthma medication, then try the test again. If your lung function improves after using the inhaler, you may have asthma.
Because asthma symptoms aren’t apparent all the time, clinicians sometimes use a challenge test to check for asthma. During this test, the patient inhales a medicine that narrows the airways. (Don’t worry–a professional will be with you the whole time). If your spirometry measurements function drop during a challenge test, you might have asthma.
A chest x-ray doesn’t diagnose asthma, but one may be ordered to look for other chest problems.
Drugs & Treatment
There is no one-size-fits-all treatment for asthma. Your clinician will work with you to determine what combination of medications and lifestyle interventions best control your asthma. It may take time to figure out what works best for you, but the effort is worth it.
Many different medications are available to control asthma. Some are taken every day; these medications are “controllers,” helping to maintain lung function and prevent asthma flare-ups. Others are so-called “rescue inhalers,” taken for sudden or persistent symptoms and used to open the airways and restore normal breathing.
Some medications that are commonly used to treat asthma include:
Bronchodilators
A medication that dilates–or opens–the airways is called a bronchodilator. Bronchodilators improve asthma by making it easier for air to flow in and out of the lungs.
Bronchodilators are usually inhaled medications. You breathe them into your airways through your mouth. The medicine comes in an inhaler; your provider will show you exactly how to use your inhaler. Proper use of the inhaler ensures that the medication gets to where it is needed–the airways in your lungs.
There are two main kinds of bronchodilators: long-acting and short-acting. Long-acting bronchodilators are “controllers” used as part of an overall management plan and usually taken daily. Short-acting bronchodilators are for “rescue,” working very quickly, and used most often used during asthma attacks or before activities that normally trigger asthma symptoms.
Antiinflammatories
“Antiinflammatory” medications are “controllers,” reducing irritation, swelling ,and production of mucus in the airways.
Corticosteroids, or “steroids,” are the most common antiinflammatory medicines used to treat asthma. These medications are NOT the “steroids” that some athletes and bodybuilders use to increase muscles. Rather, they work to control inflammation. They can be inhaled or taken by mouth, and usually every day as part of an asthma control plan. Oral corticosteroids may be prescribed for a short time, especially during times of illness or when your asthma is difficult to control.
Combination Medicines
Some inhalers contain both bronchodilators and corticosteroids. They can be useful for patients who need both kinds of medication.
Antibiotic and Antiviral Medicines
Ordinary colds and upper respiratory infections can make asthma worse. Antibiotics don’t work for viral infections like the common cold, but you may get a prescription for an antibiotic if your clinician suspects a bacterial infection that is making your asthma worse.
Your provider will review with you what medication is prescribed and exactly when and how to take it. Your pharmacist can help you with this information too.
Vaccinations
Asthma increases your chances of getting seriously ill from lung infections. That’s why health-care providers strongly recommend the influenza (flu) vaccine and pneumonia vaccine to everyone with asthma. These vaccines reduce your risk of getting influenza and pneumonia.
According to the Centers for Disease Control and Prevention, everyone with asthma who is 6 months of age or older should get a flu vaccine every year. A vaccine to prevent the most common form of pneumonia is also recommend for everyone with asthma over the age of 19 years. Ask your doctor if you’re due for a vaccination for influenza or pneumonia.
Lifestyle & Home Remedies
You can keep your asthma under control by avoiding asthma triggers, following your action control plan, and carefully tracking your symptoms.
Avoid Triggers
It’s important to know your asthma triggers. Everyone with asthma should keep his or her home clean and mold-free. If pollen triggers your asthma, stay inside as much as possible during times of high pollen counts, keep your windows closed, and use air conditioning to stay cool, if possible.
Your clinician will help you determine your asthma triggers and give you some ideas as to how you can minimize your exposure. It’s OK to ask for ideas too. If your clinician tells you that dust or dust mites trigger your asthma, ask what you should do to control your exposure to dust and dust mites. Of course, avoiding smoking and exposure to secondhand smoke is very important.
Follow your Asthma Plan
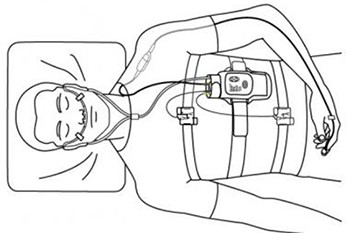
Your clinician will create an asthma action plan that’s tailored to you. It will tell you which medications you should take when and under what conditions. Your asthma action plan might ask you to monitor your lung function at home with a peak flow meter. If so, your clinician will show you how to use it, how to measure and record your lung function, and what you should do when your lung function is at various levels. You might be instructed to start a medication, for instance, when your lung function drops below a certain level.
Ask for a written copy of your asthma control plan. Make sure you understand it. Ask questions if you don’t! Give a copy of your asthma action plan to a close family member and all of your health-care professionals. If your child has asthma, make sure the school and all care providers have a copy of the asthma action plan and know how to use it. Some children with asthma qualify for an Individualized Educational Plan (IEP), so ask if this is appropriate for your child.
Track your Symptoms
Your treatment plan may need to be tweaked from time to time, depending on your symptoms. Pay attention to when, where, and under what circumstances you experience symptoms. Keep track of when (and how often) you use your rescue inhaler or other as-needed asthma medication. Write this information down, and share it with your doctor.