 Sleep Study Diagnosis in Nashik
Sleep Study Diagnosis in Nashik
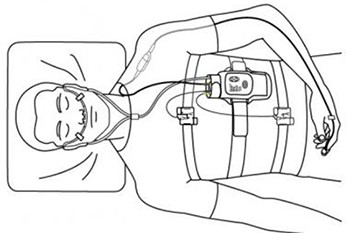
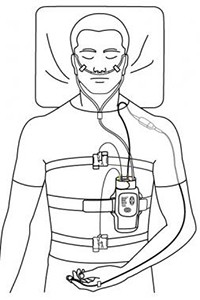
Nocturnal, laboratory-based polysomnography (PSG) is the most commonly used test in the diagnosis of obstructive sleep apnea syndrome (OSAS). It is often considered the criterion standard for diagnosing OSAS, determining the severity of the disease, and evaluating various other sleep disorders that can exist with or without OSAS. PSG consists of a simultaneous recording of multiple physiologic parameters related to sleep and wakefulness.
PSG can directly monitor and quantify the number of respiratory events (ie, obstructive, central, or complex) and the resultant hypoxemia and arousals related to the respiratory events or even independent of the respiratory events.
A single-night PSG is usually adequate to determine if OSAS is present and the degree of the disorder. However, night-to-night variability may exist in patients who have a high probability but a low apnea index. In addition, variability in laboratory equipment, scoring technique, and interscorer reliability may also play roles. As is well known, PSG scoring also usually varies from laboratory to laboratory.
PSG is used to evaluate abnormalities of sleep and/or wakefulness and other physiologic disorders that have an impact on or are related to sleep and/or wakefulness.
Parameters Monitored
Assessment of sleep stages requires 3 studies: electroencephalography (EEG), electrooculography (EOG), and surface electromyography (EMG).
One EEG channel (central channel with an ear reference provides the best amplitude) is used to monitor sleep stage. However, most laboratories use 2 central channels and 2 occipital channels, with ear references as an adjunct to help identify sleep latency and arousals. A 10- to 20-electrode placement system is used to determine the location of these channels. Additional EEG channels can be used, particularly in patients with epilepsy (ie, a full 10-20 montage).
Two EOG channels are used to monitor both horizontal and vertical eye movements. Electrodes are placed at the right and left outer canthi, one above and one below the horizontal eye axis. The electrodes pick up the inherent voltage within the eye; the cornea has a positive charge and the retina has a negative charge. Evaluation of the eye movements is necessary for 2 reasons. First is for documentation of the onset of rapid eye movement (REM) sleep, and second is to note the presence of slow-rolling eye movements that usually accompany the onset of sleep.
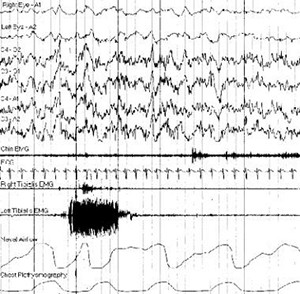 One EMG channel (usually chin or mentalis and/or submentalis) is used to record atonia during REM sleep or lack of atonia in patients with REM-related parasomnias. To assess bruxism, the EMG electrodes can be placed over the masseter. The EMG recording from other muscle groups is assessed for other sleep disorders. For example, the anterior tibialis EMG is helpful for assessing periodic limb movements during sleep and the intercostal EMG is used as adjunctive help for determining effort during respiratory events.
One EMG channel (usually chin or mentalis and/or submentalis) is used to record atonia during REM sleep or lack of atonia in patients with REM-related parasomnias. To assess bruxism, the EMG electrodes can be placed over the masseter. The EMG recording from other muscle groups is assessed for other sleep disorders. For example, the anterior tibialis EMG is helpful for assessing periodic limb movements during sleep and the intercostal EMG is used as adjunctive help for determining effort during respiratory events.
Two channels are used for monitoring airflow. One thermistor channel (oral and/or nasal) is used to evaluate the presence or absence of airflow. Any change in temperature as a patient inhales and exhales leads to a normal signal, so this channel is insensitive for partial flow obstruction. Thermistor is the recommended channel for evaluation of apneas. Nasal pressure transducer channel is a more sensitive measure of airflow restriction. Normal breathing has a rounded pattern, while resistance to airflow leads to a squaring off of the flow signal. Pressure transducer is the recommended channel for evaluating hypopneas. It is also used for airflow resistance in upper airway resistance syndrome.
Other parameters that can be monitored in a sleep study include the following :
- Electrocardiography.
- Pulse oximetry.
- Respiratory effort (thoracic and abdominal).
- End tidal or transcutaneous CO 2.
- Surface EMG monitoring of limb muscles (to detect limb movements, periodic or other).
- Continuous video monitoring.
Respiratory Events and Leg Movement Scoring
Basic rules : See the list below
- All respiratory events counted are at least 10 seconds in duration.
- All events need to have at least a 3% or greater oxygen saturation (SaO 2) decrease.
- EEG arousals occur with most respiratory events.
Obstructive apnea : See the list below
- Greater than 90% reduction in oronasal thermistor amplitude for more than 10 seconds.
- At least 90% of the event’s duration meets the amplitude reduction criteria.
- Often associated with increasing respiratory effort; usually seen as paradoxical.
- Often associated with desaturations.
Hypopnea : See the list below
- AASM recommendation (Medicare definition).
- Reduction in nasal pressure amplitude by greater than 30% lasting for at least 2 breaths.
- SaO2 of at least 3% from pre-event baseline or an arousal.
- Obstructive hypopneas can be scored if any of the following are present: Snoring, increased inspiratory flattening of the nasal pressure, or associated thoracoabdominal paradox during the event but not pre-event.
- Central hypopneas can be score if none of above findings is present.
- AASM alternative definition.
- Reduction in pressure amplitude greater than 50% of baseline value.
- SaO2 decrease of greater than 3% or arousal.
Mixed apnea : See the list below
- Greater than 90% reduction in thermistor flow for greater than 10 seconds.
- Total absence of respiratory effort at the beginning of the event, followed by a gradual increase in effort, which eventually breaks the apnea (usually paradoxical).
- SaO 2 decrease of greater than 3%.
Central apnea : See the list below
- Greater than 90% reduction in thermistor flow for greater than 10 seconds.
- Complete absence of respiratory effort.
- SaO 2 decrease of greater than 3%.
Respiratory effort–related arousal : See the list below
- Greater than 10 breaths with increasing respiratory effort or flattening of the nasal pressure followed by an arousal.
- Does not meet criteria for hypopnea or apnea.
Cheyne-Stokes respiration : See the list below
- At least 3 consecutive cycles.
- Cyclical crescendo and decrescendo change in breathing amplitude.
- Either 5 per hour of sleep or duration greater than 10 minutes.
- Typical cycle length is 60 seconds.
Sleep-related hypoventilation : See the list below
- More than 25% of the total sleep time has CO 2 >50 mm Hg.
- Measured by either end-tidal or transcutaneous CO 2 sensor.
Periodic limb movement : See the list below
- Each jerk more than 0.5 seconds but less than 10 seconds in duration.
- Minimum amplitude is an 8 mV increase in EMG voltage above resting EMG.
- Must have 4 jerks separated by no less than 5 seconds and no more than 90 seconds.
- No associated respiratory event within 0.5 seconds.
EEG arousal : See the list below
- Abrupt shift of EEG frequency including alpha, theta, and/or frequencies greater than 16 Hz (but not spindles).
- Greater than 3 seconds of changed frequency on EEG.
- At least 10 seconds of stable sleep preceding the change.
- In REM sleep, increase in submental EMG for at least 1 second.
Bruxism : See the list below
- At least twice the amplitude of baseline chin EMG activity.
- At least 3 elevations of 0.25-2 seconds of increased chin EMG activity.
- One elevation of greater than 2 seconds of increased chin EMG activity.