Who should have a spirometry?
If you answer yes to any of the following question you should ask your doctor about having a spirometry test.
- Do you (now) or have you ever smoked?
- Are you short of breath, more often than other people?
- Do you have a cough that does not go away? For example: daily coughing or the ‘morning’ cough?
- If you cough, do you cough up mucus?
- Do people around you smoke?
- Do you work around chemicals and dust?
- Does bronchitis or emphysema run in your family?
- Do you wheeze (a whistling or squeaky sound when you breathe)?
What does a spirometry tell my doctor?
 Spirometry is a simple breathing test, that can be done in physician’s office that measures the amount of air you can blow out after you have taken in the deepest breath you can. The results of this test give two important numbers that measure airway obstruction.
Spirometry is a simple breathing test, that can be done in physician’s office that measures the amount of air you can blow out after you have taken in the deepest breath you can. The results of this test give two important numbers that measure airway obstruction.
FVC – Forced Vital Capacity : the total volume of air you can forcefully blow out. It is an assessment of the size of your lungs, how well your lungs expand and contract, and how well the air passages open and close.
Patients with obstructive lung disease usually have a normal or only slightly decreased vital capacity. A Reduced FVC is associated with restrictive lung disorders, diseases that may be caused by inflammation or scarring of the lung tissue (interstitial lung disease) or by abnormalities of the muscles or skeleton of the chest wall.
FEV1 – Forced Expiratory Volume : is the volume of air that you can blow out in the first second of exhalation.
Typically FEV1 is considered “normal” if greater than 80% of predicted. FEV1 is reduced in both obstructive and restrictive lung disease.
FEV1/FVC : This ratio compares the volume of air expelled in the first second to the total volume expelled.
In healthy patients the FEV1/FVC is usually around 70%-80%. In patients with obstructive lung disease FEV1/FVC decreases and can be as low as 20-30% in severe obstructive airway disease. Restrictive disorders have a near normal FEV1/FVC ratio.
What you need to do before the test?
- Wear comfortable clothing.
- Ideally you should not use your inhalers before your spirometry. There are different types of bronchodilators; some are long acting and others are short acting inhalers so ask your doctor how long you should avoid using your inhaler/s before the test.
- If you experience breathing problems before your test, go ahead and use your inhaler/s. Inform the person performing the test the name of the inhaler/s you used, dosage/puffs taken, and the time you used them.
What happens during the test?
- You will be asked several questions (listed below) that will be used to determine what ‘normal’ lung values would be for you if your lungs were healthy.
- Age : lung function declines with age.
- Height : taller people have larger lungs.
- Sex: women have smaller lung volumes.
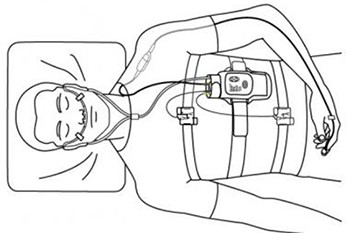
- You will be asked to sit up straight and uncross your legs or to stand up.
- Often you will have a nose plug placed on your nose.
You will be instructed to :
- Take in a big breath.
- Place the mouthpiece into your mouth and seal your lips tightly around the mouthpiece.
- Blast your air into the mouthpiece as hard and fast as you can, squeezing out all the air in your lungs.
- Keep on blowing out the same breath until you are told to stop.
- To make sure you understand the directions ask the technician to demonstrate the procedure.
- The test will be repeated several time to make sure that the measurements are correct.
- The spirometry may be repeated after you receive a bronchodilator inhaler or nebulizer.