Thoracoscopy
What is LAVAT?
Local Anaesthetic Video Assisted Thoracoscopy (LAVAT), also known as medical thoracoscopy, is a minimally invasive diagnostic and therapeutic procedure used to assess pleural diseases and pleural fluid collections. Performed under local anaesthesia and conscious sedation, LAVAT allows for direct visualization of the pleural space, facilitating safe biopsies, fluid drainage, and pleurodesis. It is typically a day-care procedure performed in a hospital setting.
Why Choose LAVAT?
LAVAT offers many benefits over more invasive options like VATS (Video Assisted Thoracoscopic Surgery):
Less invasive with minimal incisions
Lower anaesthetic requirement
Reduced complications such as re-expansion pulmonary oedema
Accurate pleural biopsies and effective pleurodesis using talc
Rapid recovery and outpatient management
LAVAT in Nashik is especially useful when previous ultrasound-guided thoracentesis has not yielded a diagnosis.
Who is Suitable for LAVAT?
LAVAT is ideal for patients with:
Undiagnosed pleural effusion despite previous testing
Need for pleural biopsy or pleurodesis
Conditions unsuitable for general anaesthesia or surgical thoracoscopy
However, it is not recommended where extensive thoracic surgery is indicated.
Procedure Overview – What to Expect
LAVAT is often done under conscious sedation, although some cases may require short hospital admission. Here’s how the procedure unfolds:
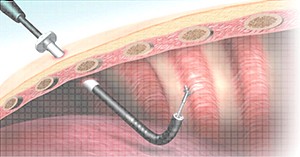
Patient is prepped and positioned.
A small incision is made to insert the pleuroscope.
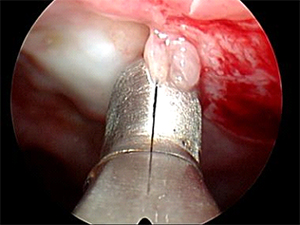
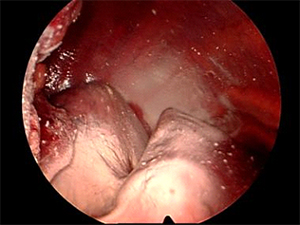
Pleural fluid is drained, and pleural surfaces are inspected.
Biopsies are taken under direct vision.
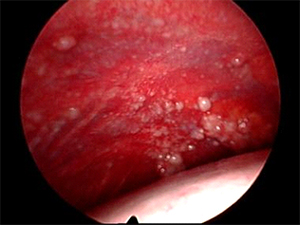
Talc may be insufflated to perform pleurodesis, preventing fluid recurrence.
The procedure is generally well-tolerated, with minimal discomfort.
History of Thoracoscopy
Thoracoscopy was pioneered in 1910 by Hans-Christian Jacobaeus in Sweden. Initially used for treating tuberculosis, the technique evolved through the decades. Today, medical thoracoscopy (LAVAT) is performed by pulmonologists using advanced video-assisted technology. Surgical thoracoscopy (VATS) is still performed by thoracic surgeons, but LAVAT has become the preferred choice for diagnostic and therapeutic pleural interventions in patients who are unfit for surgery.
Medical Indications for LAVAT
LAVAT in Nashik is recommended for the following clinical scenarios:
Undiagnosed Pleural Effusion
Direct visualization of the pleura offers diagnostic accuracy greater than 90% in cases where thoracentesis or cytology fails.
Malignant Pleural Effusion
Allows therapeutic pleurodesis via talc insufflation, improving quality of life and reducing recurrence.
Lung Cancer with Negative Cytology
Enables accurate staging and avoids unnecessary surgeries.
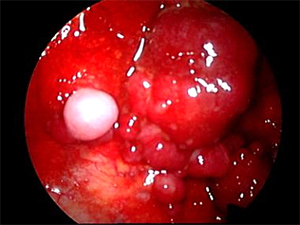
Suspected Malignant Mesothelioma
Offers superior diagnostic yield compared to cytology, especially in early detection.Tuberculous Pleural Effusion
Provides large tissue samples and facilitates drainage or adhesiolysis in select cases.Recurrent Benign Effusions
Useful for managing heart failure-related, post-surgical, or nephrotic effusions.
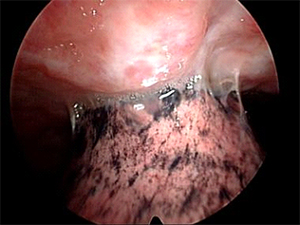
Empyema and Parapneumonic Effusions
Selected cases with thin adhesions may benefit from early thoracoscopic drainage and lysis.Pneumothorax
Offers diagnostic inspection and definitive pleurodesis in non-surgical candidates.
Contraindications for LAVAT
Absolute and relative contraindications must be carefully assessed:
Absolute: Inability to safely access the pleural space
Relative (can be managed prior to procedure):
Refractory cough
Hypoxia
Coagulopathy
Thrombocytopenia
Thoracic ultrasound can assist in identifying a safe pleural window. A minimum pleural separation of 10 mm is generally recommended.
Diagnostic Superiority of LAVAT
| Condition | Diagnostic Yield (LAVAT) |
|---|---|
| Malignant Pleural Effusion | 95% |
| Pleural Mesothelioma | >90% |
| Tuberculous Effusion (with biopsy) | Up to 88% |
Compared to thoracentesis and closed needle biopsy, pleuroscopy in Nashik offers significantly better diagnostic clarity, allowing tailored treatment.
Therapeutic Benefits of LAVAT
Talc Pleurodesis: Effective in >90% of cases
Adhesion Lysis: Improves lung re-expansion
Effusion Drainage: Better symptomatic relief
Improved Functional Status: Enhances eligibility for cancer therapies
LAVAT at Dr. Mutha Hospital – Thoracoscopy in Nashik
Dr. Mutha Hospital is among the leading centers for LAVAT in Nashik, offering state-of-the-art video-assisted thoracoscopy under local anaesthesia. We ensure:
High diagnostic accuracy
Patient comfort and safety
Personalized treatment approach
Integration of LAVAT with broader respiratory care (like Bronchoscopy in Nashik and Sleep Study Diagnosis)
Ready to get our medical care? We’re always wait for serve you, Make an Appointment.
Appointment
Our Pricing Packages
- Neurology Care
- Medical Care
- Child & Old Care
- Dental Care
- On-Time Delivery
- Neurology Care
- Medical Care
- Child & Old Care
- Dental Care
- On-Time Delivery
- Neurology Care
- Medical Care
- Child & Old Care
- Dental Care
- On-Time Delivery